|
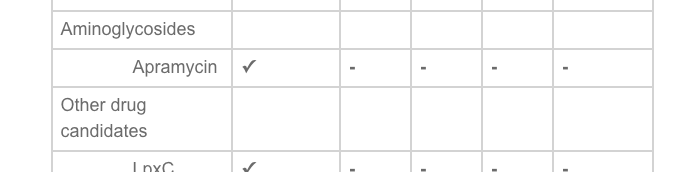
Our latest manuscript: "Synergistic combinations and repurposed antibiotics active against the pandrug-resistant Klebsiella pneumoniae Nevada strain." Antimicrobial Agents and Chemotherapy early release identifies:
Highly synergistic activity of several antimicrobial combinations. Low apramycin and spectinomycin MIC values. CDC previously reported that none of 26 antimicrobials they tested were active against the Nevada strain. That made the strain until now pandrug-resistant. Links to several news articles about this pandrug-resistant strain:: The Atlantic. NPR, NBC, PBS. Forbes
0 Comments
"New Treatment Options against Carbapenem-Resistant Acinetobacter baumannii Infections" cites our murine apramycin PK/PD studies and activity spectrum studies against "CRAB.".
New antibiotics that may offer additional and much needed treatment options will only be used in hospital systems if the clinical microbiology laboratory can provide timely antimicrobial susceptibility testing data. Historically there has been a time lag in the availability of susceptibility testing methods either at reference laboratories (long delay to results), incorporation in automated commercial systems (4 years), or simpler methods like disk diffusion and gradient strips that can be performed manually on an as needed basis. I was excited to learn that delafloxacin and meropenem/vaborbactam disk diffusion and gradient strip methods finally became available. Fantastic. However, before we can introduce those methods in the clinical laboratory, we need to validate performance of these methods per CLIA '88 regulations and good laboratory practice. This requires either comparing the new methods to a reference standard (broth microdilution -- need antibiotic powder, and a lot of set up time) or a set of strains that has been previously characterized by a reference dilution method and has a good representation of susceptible and resistant isolates. Those are serious roadblocks. By chance, I happened to give a talk at the Northeast Branch of the American Society of Microbiology and a someone from Melinta Pharmaceuticals happened to be there, and that someone referred me to our local Key Account Manager who offerred a solution "on request". Specifically, Melinta or other pharmaceutical companies are not allowed to approach me and tell me about a solution, but if I inquire independently and ask for a previously characterized set of bacterial isolates, they are allowed to tell me that in fact they have a series of previously characterized isolates for both drugs available for validation. These isolates are provided free of charge from Laboratory Specialist, Inc, Sent by FEDEX with first class documentation, data for broth microdilution performed circa ten times on each isolates with modal MICs and MIC distribution - wow, that is awesome. Methods validated beautifully. It just seems odd to me that such a valuable resource, providing clinical laboratories the ability to robustly evaluate AST methods for newly marketed drugs, needs to remain on a need to know basis. Clinical labs, please take note of this available resource. The same proved to be true for plazomicin. Achaogen uses the same Laboratory Specialists, Inc. to provide 30 characterized isolates on request; however, the FEDEX chargers are not absorbed. The FDA-CDC Biobank also now has a set of isolates characterized for plazomicin susceptibility and I see now also delafloxacin., I suspect the exact same set of organisms. The existing rule restricting such company-clinical laboratory communication about these important resources should be relaxed! We need facile access to validation strains sets to bring new testing into our laboratories in a timely fashion, to facilitate the availability of new antibiotics when they are most needed, and to help support profitability of antibiotic development by pharmaceutical companies.
Apramycin scaffold exploration using novel glycochemistry and SAR studies to enhance activity against Acinetobacter baumannii and other multidrug-resistant Gram-negative pathogens.
George O'Doherty "Research May Help Rescue Antibiotics’ Effectiveness in the Face of Drug-Resistant Bacteria"8/10/2018 BIDMC news release on Thea's antimicrobial synergy paper:
"Bacteria—especially Gram-negative strains—are becoming increasingly resistant to current antibiotic drugs, and the development of new classes of antibiotics has slowed. Faced with these challenges, investigators are studying the potential of combination therapy, in which two or more drugs are used together to increase or restore the efficacy of both drugs against a resistant bacterial pathogen. Now new research indicates that such synergy may work even when bacteria become resistant to colistin, which is considered a treatment agent of last resort. The findings are especially promising because recent evidence indicates the potential for rapid worldwide spread of colistin resistance. “For an infected patient, if the multidrug-resistant Gram-negative bacterial pathogen is resistant to colistin, then there is a big problem,” said senior author James Kirby, MD, Director of the Clinical Microbiology Laboratory at BIDMC. In their Antimicrobial Agents and Chemotherapy study, Kirby and his colleagues Thea Brennan-Krohn, MD and Alejandro Pironti, PhD screened 19 different antibiotics for synergy with colistin. The team discovered several combinations where synergy was present and infections with resistant pathogens could potentially be treated with the combination therapy. Of particular interest, colistin demonstrated high rates of synergy with linezolid, fusidic acid, and clindamycin, which are protein synthesis inhibitor antibiotics that individually have no activity against Gram-negative bacteria. “It was remarkable to see two drugs, each of which is inactive on its own against these bacteria, inhibiting them in combination,” notes Brennan-Krohn. “These findings suggest that colistin retains sub-lethal activity against colistin-resistant bacteria, which may enable drugs like linezolid to reach their targets.” “Faced with highly resistant pathogens, clinicians often currently treat with multiple antibiotics without knowing the benefit the combinations may provide,” said Kirby. “This study now provides some scientific underpinning for these choices and direction for future investigation.” He added that combination therapy may also allow clinicians to use lower effective doses of colistin and other drugs, which would help avoid toxicities associated with the medications as well as slow the development of antibiotic resistance. This work was funded in part with Federal funds from the National Institute of Allergy and Infectious Diseases, the National Institutes of Health, and the Department of Health and Human Services." Congratulations to lab members, Anthony Kang, and colleagues for our manuscript newly accepted in Antimicrobial Agents and Chemotherapy titled: "Efficacy of Apramycin against Multidrug-Resistant Acinetobacter baumannii in the Murine Neutropenic Thigh Model"
The manuscripts describes potent in vitro and in vivo activity of the apramycin, an aminocyclitol aminoglycoside, against multidrug-resistant and extensively-drug resistant Acinetobacter baumannii. In prior manuscripts, we demonstrated broad activity against several types of multidrug-resistant pathogens including carbapenem-resistant Enterobacteriaceae (CRE), Acinetobacter baumannii and Pseudomonas aeruginosa Congratulations to KP Smith on being award an NRSA F32 postdoctoral fellowship..
on Drug Development to Meet the Challenge of Antimicrobial Resistance, September 6-8, 2017. Posters were on apramycin, inkjet printer-based susceptibility testing methodology, and MAST rapid susceptibility technology, respectively.
A thoroughly enjoyable book on the history of antimicrobials. A big thanks to Thea for recommending!
|
Kirby Lab Blog Categories
All
Archives
July 2024
|
 RSS Feed
RSS Feed